Of the almost 27 million Americans with osteoarthritis, about 60 percent of them are women—and the risk of osteoarthritis shifts with age. Until age 55, more men are affected, but after age 55, the number of women with the condition surpasses the number of men. Gender also determines which joints tend to be affected by osteoarthritis. It is more common for men to experience arthritis in their hips. In women, arthritis tends to affect the hands or knees. In addition, research suggests women tend to report more severe osteoarthritis Pain. So research has proven arthritis is more common in women than it is in men. Discover why women are more susceptible to arthritic conditions.
Changes in hormone levels: Hormone levels fluctuate with menstruation cycles and change during menopause.
- Menstruation and Joint Laxity – Many women with OA, RA, lupus, and fibromyalgia report an increase in joint pain just before or during their periods. This is likely because estrogen levels plummet right before menstruation and rise again after a woman’s period is over. Ligaments throughout the body have estrogen and progesterone receptors to help with the appropriate balance of strength and flexibility of the ligaments. Estrogen causes a decrease in the cells that make collagen and other connective tissues of the ligaments, therefore making the tissues looser. the relationship between menstruation, joint laxity, and osteoarthritis is perhaps most clear in the case of knee osteoarthritis. Many researchers believe fluctuations in join laxity help explain why female athletes are 2 to 8 times more likely than men to tear the ACL in the knee.
- Menopause – Women’s risk of developing osteoarthritis increases significantly after menopause. Estrogen level drop during menopause, this drop contributes to changes in the body that accelerate the osteoarthritis process. After menopause, when women’s estrogen levels go down, they lose that protection and may have a higher risk of developing osteoarthritis even if they are on hormone-replacement therapy.
Differences in the musculoskeletal system and Biomechanics
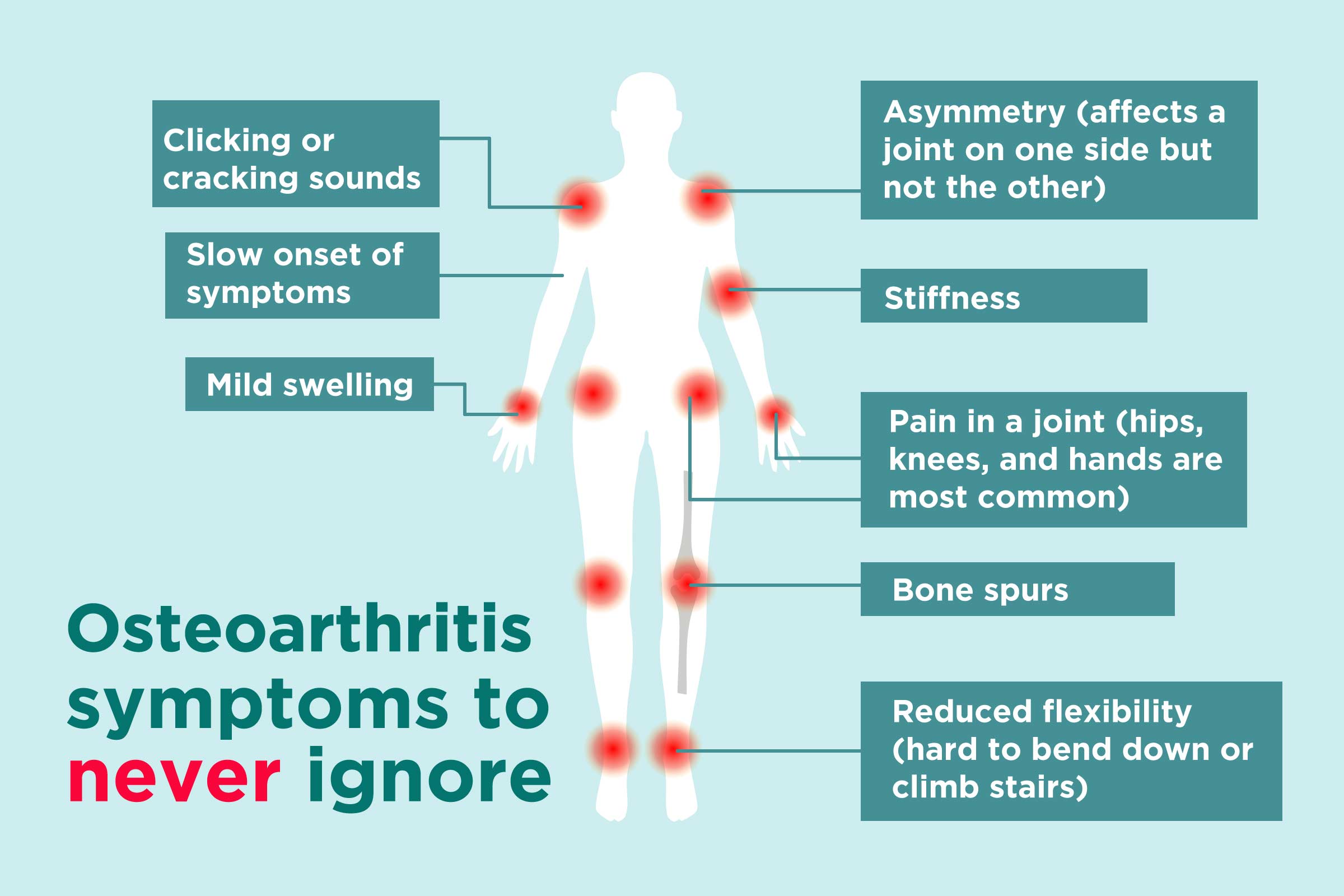
Besides the breakdown of cartilage, osteoarthritis affects the entire joint. It causes changes in the bone and deterioration of the connective tissues that hold the joint together and attach muscle to bone. It also causes inflammation of the joint lining. While women’s bodies have the same joints as men, certain musculoskeletal differences exist. These differences alter the gait and how their joint surfaces move in relation to one another (joint articulation). Because of the anatomic difference, there is evidence that women’s knees experience more wear and tear.
The Tendency to Carry Excess Weight
At menopause, many women experience weight gain, particularly around the abdomen. Contributors to weight gain at menopause include declining estrogen levels, age-related loss of muscle tissue, and lifestyle factors such as diet and lack of exercise. According to the National Institute of Health, US women are more likely to be obese than men. Obesity increases the risk of osteoarthritis. the extra weight puts more stress on the hips, knees, and ankles. This stress leads to friction between the bones and joints. Obesity may be a low-grade systemic inflammatory disease. This inflammation may contribute to the development of osteoarthritis in any joint.
Experts are still investigating why women are more likely to get osteoarthritis. The researchers found that in men with osteoarthritis there were 50 biological processes altered due to differences with the microRNAs of healthy patients, whereas in women up to 70 processes were altered. microRNAs were not recognized as a distinct class of biological regulators until the early 2000s. In the study published in the journal Scientific Reports, researchers explain that the gender differences found in synovial fluid are the key to explain why osteoarthritis affects women more. In women, they observed that microRNAs that should be sending favorable messages to the joints, such as the promotion of estrogen signaling and collagen-producing cells, were deactivated.
For persistent pain that is interfering with your daily activities, see a rheumatologist to make the correct diagnosis and begin the proper treatment.
Contact Us (859-331-3100) For More Information to Request an Appointment
—
 About Tristate Arthritis and Rheumatology
About Tristate Arthritis and Rheumatology
Tristate Arthritis and Rheumatology is first and largest Rheumatology practice in the Northern Kentucky area. Founded by Dr. Arthur Kunath in 1986, our rheumatology practice now consists of six doctors who are board certified in both Internal Medicine and Rheumatology and a Physician Assistant. Patients see one doctor (except in emergencies), thereby assuring continuity of care and an individualized doctor-patient atmosphere giving the physician the ability to establish personalized and detailed relationships. Our doctors have received numerous awards, including being listed as “Top Doctors” in Cincinnati Magazine, receiving the Patient’s Choice Award, the Most Compassionate Doctor Award, and the American College of Rheumatology’s “My Doc Rocks” award.
>> Learn More



